All About Vaginismus: When “ooooh” becomes “ouch! (Part 1)
You may not know this about me….but, treating someone who was having painful sex (specifically, vaginismus) was a pivotal moment for me in my career path as a pelvic health physical therapist. I’ve shared this story before, so skip ahead if you’ve heard it :-) But, I was in my 3rd year of PT school, on my first full-time clinical rotation. We evaluated a patient who was experiencing pain with sexual intercourse. In fact, she was in tears during her initial evaluation, as she had a history of several relationships ending due to her inability to have sex without pain. Initially, when we examined her, she had significant pain with even the tip of a finger inserted into the vagina. One day, after several visits, she came into her appointment, sat down, and started crying. When we asked her what was going on, she just said, “I had sex… and it didn’t hurt.” It gave me goosebumps then. It gives me goosebumps now. And it was a moment for me. At that minute, I said to myself, “I have to help these people.” I changed my path. Switched my plans for specialization. And I have never looked back!
Pain with sexual intercourse impacts a significant number of individuals. In fact, it is thought to impact around 20% of individuals worldwide. Vaginismus is a condition where a person experiences pain with insertion into the vaginal canal. This could be during sexual intercourse, but may also occur with the use of tampons, or during pelvic medical examinations. This pain is accompanied by muscle spasm of the pelvic floor muscles, particularly, the superficial layer of the pelvic floor.
Let’s Meet the Pelvic Floor Muscles
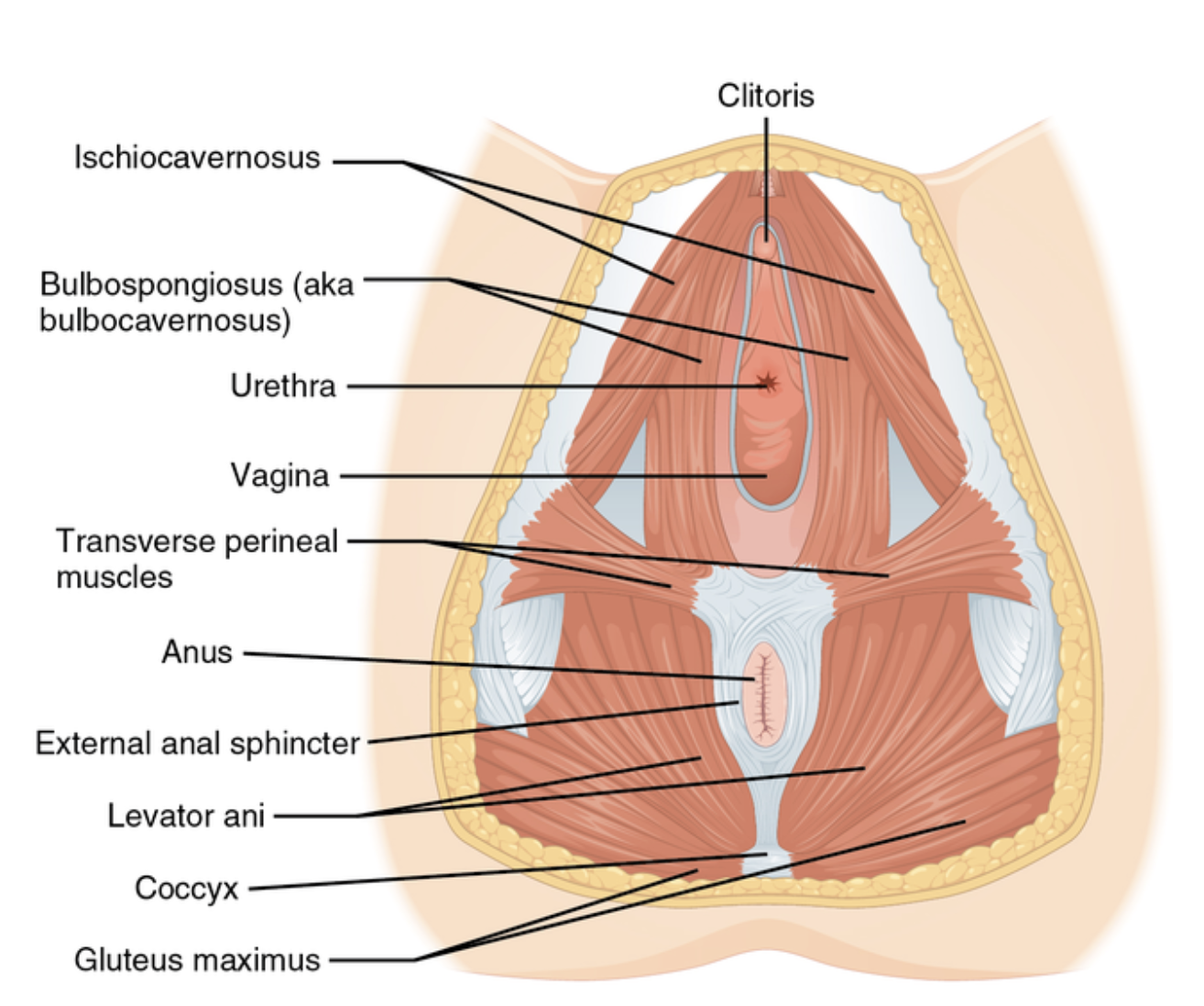
The pelvic floor muscles are composed of 3 layers of muscles, and run inside the bottom of the pelvis, from the pubic bone in the front, to the tailbone in the back. The deepest layer of the muscles hold the ever-popular levator ani– a group composed of pubococcygeus (and puborectalis) and iliococcygeus. These muscles lift the anus for bowel continence and provide support to the organs. Also, in this layer is coccygeus, which attaches to the tailbone (and would let us wag our tail if we were puppies!).
Moving toward the front, we have our second layer. This layer has several muscles that run around the urethra, and help aid in bladder control, and a muscle called sphincter urethrovaginalis, which helps to close the urethra and the vagina.
Then, we reach our first layer, the most superficial layer. This layer includes the bulbospongiosus, which attaches to the covering of the clitoris and loops around the vagina, and also the ischiocavernosus, attaching along the pubic ramus (bone) and attaching to the covering of the clitoris. It also includes the superficial transverse perineal muscle (running from your sit bones across the perineal body– the area between the vulva and anus) and the external anal sphincter.
Check them out in the image below:
The pelvic floor muscles have several very important jobs for us. They help us control our bladder and bowel movements. They provide postural stability and organ support. They aid in breathing, blood and lymphatic flow. And, they help with sexual function. This includes contracting to pull blood into the clitoris (or penis) for arousal, rhythmic contractions for orgasm– and, lengthening to allow for sexual insertion.
When a person experiences vaginismus, they will have pain accompanied by muscle spasm/guarding with insertion into the vaginal canal. This could be with using a tampon, having a medical examination, or with sexual insertion. Typically, we find that the muscle tension is most significant at the superficial layer of the pelvic floor muscles. Some patients will descirbe this as feeling like their “vagina just closes” or that their partner “hits a wall.”
What causes vaginismus?
It’s complicated, honestly. We know there are factors that might play a role. Things like:
Childbirth (injuries like tears, etc can contribute)
Prior pelvic surgeries
Difficult/painful pelvic procedures
Prior yeast or bacterial infections
Prior trauma (physical, emotional, sexual)
Prior difficult or painful medical examinations or sexual experiences
Guilt/shame around sex
Anxiety
But, the reality is that sometimes we really can’t pinpoint a specific cause or factor involved.
The complex role of the brain in all of this
So far, we’ve focused on the muscular components when a person is experiencing pain like this, and some of the known factors or causes that could be involved. However, the muscles are just one piece of the puzzle. I always tell my patients that their brains are very smart. When something has been shown to be painful, the brain can start to build patterns– increase the sensitivity of certain pathways– and build predictions. This is protective to us, and makes a lot of sense. If I know that touching a hot stove is painful, I’m going to be more careful around the stove. I’m going to proceed with caution, and make sure it isn’t hot before I touch it. When every sexual interaction leads to pain (and this pain can often be very emotionally taxing as well!), it makes sense that the brain will start to guard and protect. Some of my patients realize that they may start feeling anxious when they know a sexual encounter is possible. Some will begin avoiding relationships. Some start to feel themselves brace when a partner even hugs them. These are normal neural adaptations when something has become painful. And the great news is that we have lovely approaches to help retrain the nervous system while we’re addressing what is happening with the muscles.
I really could go on and on about this piece– but instead, I’m going to link you to some additional reading items if you’d like to explore the further. So, check these things out:
There’s a Pelvis in Your Brain
Your Brain is Playing Tricks on You: Part 1 - Visual Illusions
Your Brain is Playing Tricks on You: Part 2 - Pain
Your Pelvic Floor as a Threat-o-meter
If you think this sounds a lot like you, you’re not alone. Remember, vaginismus impacts around 2-6% of people and nearly 20% have pain with sex.
So, let’s move on to what should happen in the search to get help.
The Medical Exam
Ok, let’s debunk a few myths. First, the medical exam should not be painful. It can feel like pressure. But pain? Nope. So, if you have pain when your provider inserts a speculum, speak up. Let them know it is happening. They should pay attention to that– explore why it is happening for you– and offer you options for solutions to that pain.
The medical examination is very important as there are multiple factors that can contribute to pain with examination/tampon use/sex. This can include:
Skin conditions (ie lichen sclerosus, etc)
Yeast, bacterial, fungal infections
Problems with the cervix or uterus (ie fibroids)
Endometriosis
Hormonal challenges (ie vaginal dryness due to genitourinary syndrome of menopause)
Sexually transmitted infections (STI’s)
Vulvodynia
… and more!
For this reason, being appropriately medically examined is crucial. This includes taking a thorough medical history, examining the skin and external tissue, examining the abdomen and pelvis, and an internal vaginal and pelvic examination. Following the exam, the provider may recommend additional testing like labs, ultrasounds, or imaging, if that is indicated.
A few notes on the medical examination
Unfortunately, education and knowledge on pelvic pain and painful sex varies significantly. Some providers are excellent– however, I have seen many patients who have experienced providers that clearly were not appropriately trained in addressing this sort of pain.
That being said, please know that 1) Informed consent is a RIGHT that you have, and should be an on-going process. 2) If an exam is becoming uncomfortable, you have every right to stop the exam at any time– and your provider should respect that. 3) “forcing” a speculum in or “just getting through it” does NOT tend to fix vaginismus. In fact, it can create a new trauma, cause severe pain, and be extremely problematic– regardless of what your provider may be telling you.
You also have every right to refuse a speculum examination if you do not feel ready for that or have had difficult experiences with that in the past. A well-trained and compassionate provider will respect that and work with you to find the best examination strategy FOR you.
Your pain is real. So, if your provider makes you feel anything other than validated for seeking help– you need a new provider.
Soooo, we’re going to shift gears now and chat about physical therapy. What should the best physical therapy initial evaluation look like? What about treatment? Stay tuned for Part 2!!