A Pain in the Tail...bone (Part 1- What is it? How does it happen? How does it feel?)
Let me tell you a little story. Several years ago, I was on my way to a continuing education course in Minneapolis, MN. I arrived to the airport early for my flight and settled in at the gate with a good book waiting for the boarding call. My flight was delayed...and delayed... a one hour wait became a four hour wait. But, I was reading a great book. I believe I got up one time over those four hours. Then I boarded the plane and sat for another 3 hours (finished the book!). Then I had tailbone pain.
Thankfully, in my case, I was headed to a course full of pelvic health practitioners, and I begged one of them to treat my tailbone on the first day. (Yes, it literally went, "Hi, my name is Jessica, will you treat my coccyx?") She did, and one day later it felt totally better.
The truth is, my story is not a totally uncommon one. I sat in one place for 7 hours straight (likely in a slumped posture)-- and my tailbone didn't like it. I was lucky, because I know about tailbone pain...I was able to get it treated and I got better very quickly. Many people with the same pain will stay in pain for a long time before getting the treatment that helps. So, my goal today is to tell you exactly what tailbone pain is, how it happens, and what it feels like... and then in part 2 to tell you what you can do about it.
First, where exactly is the tailbone? Seems easy, but you'd be surprised how many people don't actually know where it is. Several months ago, I received a referral from a PT colleague to treat a nice lady who was having "tailbone pain." She came into my office and when I asked where her pain was, she pointed directly to the sacrum. I have had this happen in reverse too where a patient told me his "back hurt" but pointed to his coccyx. So, where is the tailbone?
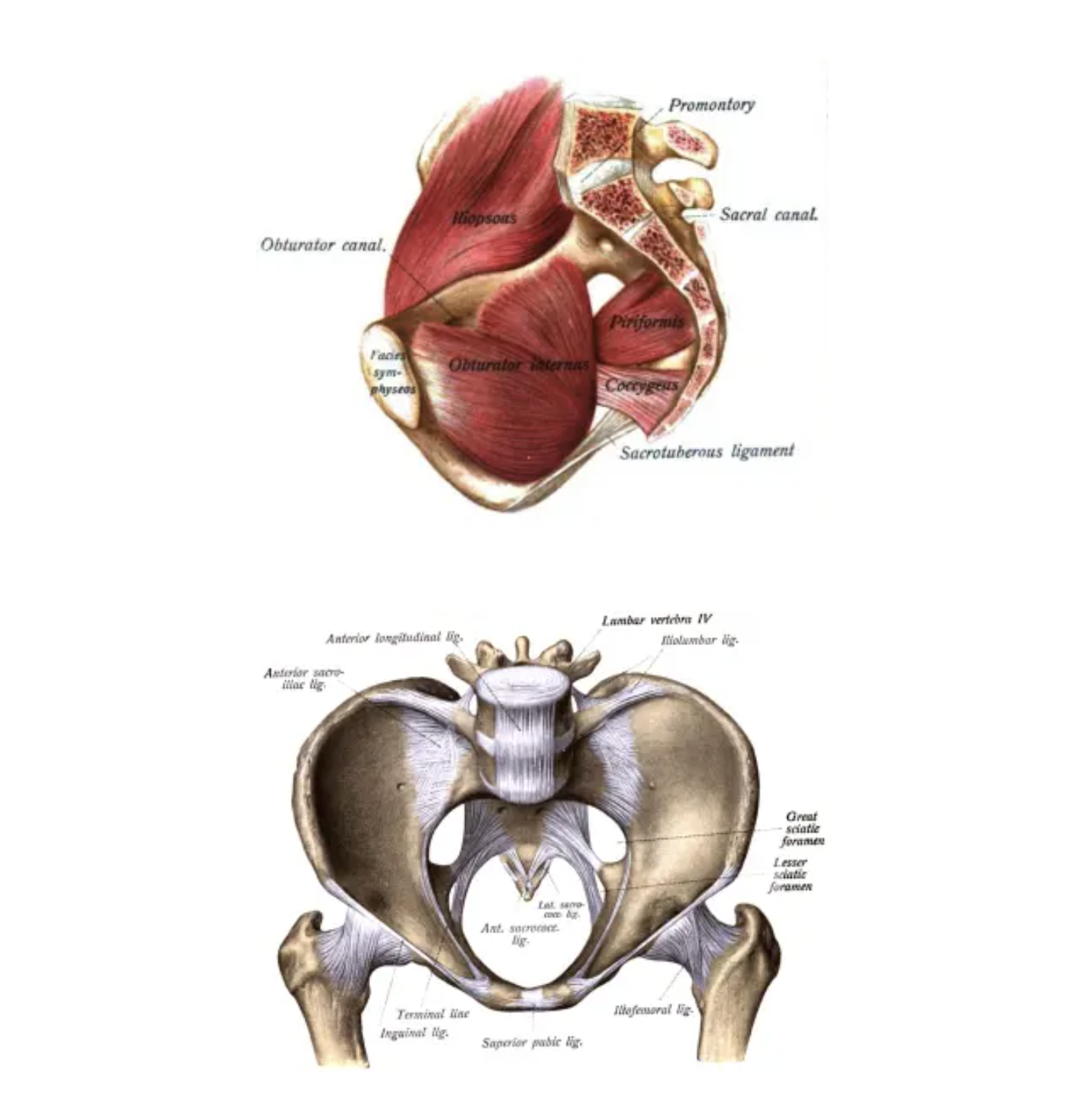
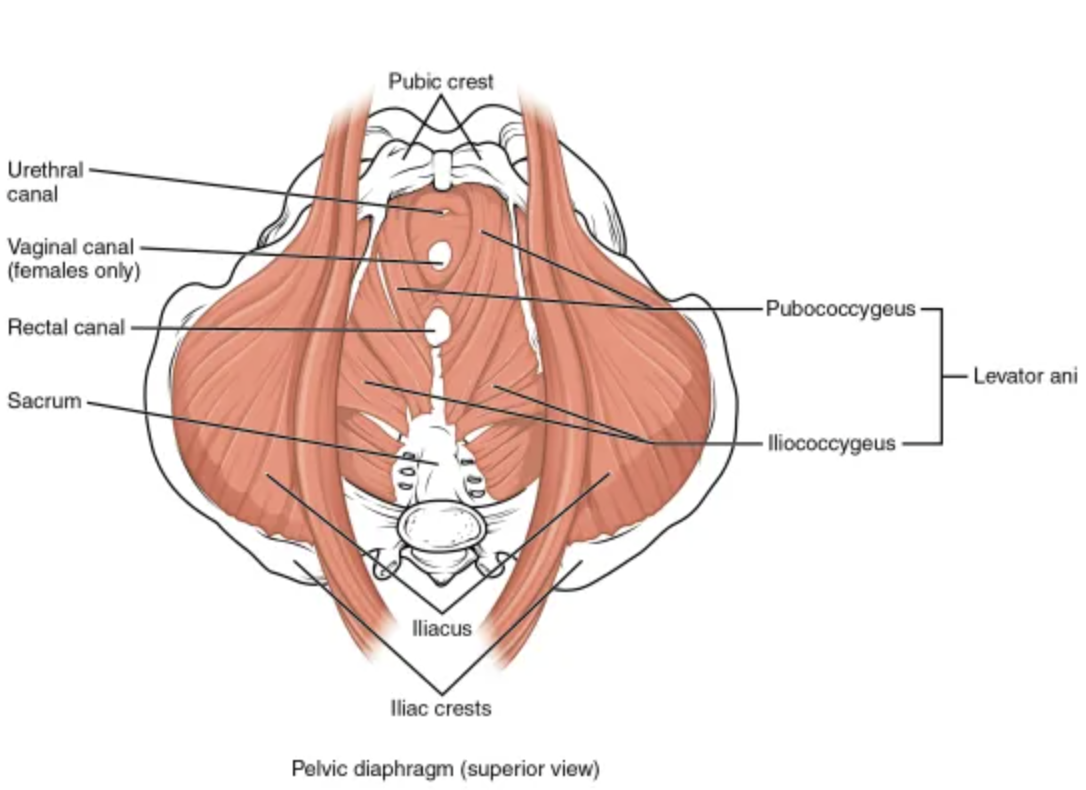
The coccyx (tailbone) refers to the 3-5 fused bones at the very end of the spine. These fused segments attach to the sacrum. To feel your coccyx, slide your fingers down from the sacrum between each cheek of your bottom. You will feel a very small boney structure, and can often feel the tip of the coccyx (which will be very close to the anus!).
Several ligaments and muscles attach to the coccyx, including the gluteus maximus and the pelvic floor muscles. The coccyx does not stay still when we move. In fact, the coccyx moves as we sit and moves again as we stand.
Now that we got that out of the way, here are a few things to know about coccydynia (tailbone pain):
-What is it and what are the common symptoms associated with it? Coccydynia translated means "pain in the coccyx," and that is how coccydynia is defined. Most people with coccydynia will complain of pain in sitting (especially on hard surfaces), pain in standing for a long period, and pain when moving from sitting to standing or from standing to sitting. Since the pelvic floor muscles attach to the coccyx, many people with coccyx pain will have pelvic floor muscle involvement to some extent and may complain of constipation or pain with bowel movements, changes in urinary frequency/urgency or pain with sexual intercourse. Clinically, I also will often find that people with tailbone pain will begin to have low back pain too-- I believe this occurs as people alter sitting positions and "side-sit" to avoid sitting on the tailbone.
-How common is it? The prevalence is actually unknown. Some literature state that it is "uncommon," but I don't really think that's true. I think it's likely under-reported (as are many things in the pelvis), and I believe the lack of understanding on treatment options contributes to this. Coccydynia seems to affect women more than men (5x more approximately!) and is more common in people with obesity.
-What causes it? Coccyx pain is typically divided into two categories-- traumatic and non-traumatic. Traumatic coccydynia typically occurs either with a backwards fall on the bottom or during childbirth. In these cases, the coccyx can become bruised, dislocated or even fractured. Nontraumatic coccydynia can occur due to prolonged or repetitive sitting on a hard surface (microtrauma), hypomobility or hypermobility of the coccyx (basically, the tailbone isn't moving properly), degenerative joint or disc disease, and other variations in the structure of the coccyx. In addition, the coccyx can sometimes become painful if a person has overactive pelvic floor muscles as these muscles attach to the coccyx. Note: Although much less common, coccyx pain can sometimes come from more serious problems like an infection or even cancer. It's always important to see a skilled health care provider who can help you determine the contributors to your pain.
-How is coccydynia diagnosed? As I said previously, coccydynia refers to pain in the coccyx, so the best way to diagnose coccyx pain is with a thorough history of the pain and an exam involving touching the coccyx to determine if it is uncomfortable to the person. (This is where some clinicians run into issues...you see, the tailbone is close to the anus, and people don't always like going there. But it is SO important as a clinician to actually touch the tailbone to help determine why the person is experiencing pain! No one would examine shoulder pain without touching the shoulder! So, please clinicians, palpate the tailbone. Soapbox over.)
I know you would think that most people would "know" if their tailbone was painful...but like we discussed above, many people do not even realize where the tailbone is! Also, it is important to note that tailbone pain can be radicular in nature, meaning that nerves in the area are contributing to the symptoms or it can be "referred pain" meaning that it is coming from a different structure. Some of the muscles that can contribute to tailbone pain are the pelvic floor muscles, the obturator internus ( a deep hip rotator) and the gluteus maximus. I have seen several patients that felt pain in their tailbone that was actually coming from tenderness in these muscles. That's why an exam with palpation is so important.
- How is the coccyx examined? Examination with a physician typically will include a subjective history, physical exam and may also include some type of diagnostic imaging (x-ray, MRI). Typically, when a person comes into my office seeking physical therapy for coccydynia or tailbone pain, my initial assessment includes the following:
A comprehensive history to understand what the person believes is causing the pain, what makes pain better/worse, obstetric history, bladder/bowel history and symptoms, sexual history and symptoms
A movement exam- basically taking a person through movements of the spine, sitting, standing, squatting to see how the person moves and what movements (if any) bring on the pain, worsen it, or alleviate it. I also will feel the coccyx in sitting vs. slumping to feel the movement of the coccyx and identify pain.
An external assessment of the spine- Mobilizing the segments of the low back, the sacrum and then the coccyx helps me identify which structures may be involved in the person's discomfort.
An external muscle assessment- feeling the muscles of the low back, buttocks, pelvic floor and thighs to see if the muscles are tender and if that tenderness contributes to tailbone pain.
An internal assessment of the pelvic floor muscles and coccyx- For patients experiencing significant pain, I will often defer this to the 2nd visit or even later depending on the person. The best way to assess the coccyx is by an internal rectal assessment by a very skilled practitioner. This examination allows a clinician to feel the movement of the coccyx and assess the muscles around the coccyx for tenderness. (Note: examination and treatment should always be a "team" decision. If a person feels uncomfortable with an internal exam and does not wish to have one, the practitioner should respect that and treat the person as well as she can with external approaches)
How is tailbone pain treated and what can you do NOW to make it better? Stay tuned next week for Part 2... :)
As always, I love to hear from you! Please let me know if you have any questions or comments! Happy Friday!
~ Jessica